 Women typically undergo an ultrasound at their gynecologist’s office as part of the evaluation process to determine the presence of uterine fibroids. Although useful, ultrasound is a rudimentary imaging tool for fibroids that often does not show other underlying diseases or all of the existing fibroids. For this reason, MRI is the standard imaging tool used by interventional radiologists for pre-procedural evaluation.
Women typically undergo an ultrasound at their gynecologist’s office as part of the evaluation process to determine the presence of uterine fibroids. Although useful, ultrasound is a rudimentary imaging tool for fibroids that often does not show other underlying diseases or all of the existing fibroids. For this reason, MRI is the standard imaging tool used by interventional radiologists for pre-procedural evaluation.
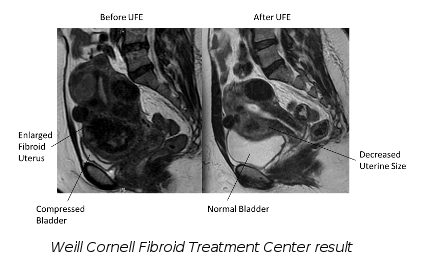
Magnetic resonance imaging (MRI) improves the patient selection for who should receive nonsurgical uterine fibroid embolization (UFE). Interventional Radiologists can use MRIs to determine if a fibroid can be embolized, detect alternate causes for symptoms, and identify pathology that could prevent a woman from having a UFE, thus avoiding ineffective treatments. Using an MRI rather than ultrasound is like listening to a digital CD rather than a cassette tape – the quality is better in every way. By working with a patient’s gynecologist, Interventional Radiologists can use MRIs to enhance the level of patient care through better diagnosis, better education, better treatment options and better outcomes.
For true informed consent before surgery, patients should be aware of all of their treatment options. Patients should get a second opinion from an Interventional Radiologist, who is most qualified to interpret the MRI and determine if they are candidates for UFE.

